Out-of-Network Benefits: What They Are, Why They Matter, and How to Use Them for Therapy
When it comes to starting therapy, most people begin with the question: “Do you take my insurance?” It’s an important question—but not the only one you should ask. Even if a therapist isn’t on your insurance company’s “in-network” list, you may still have out-of-network (OON) benefits that can make therapy more affordable than you realize.
Here’s what out-of-network benefits are, why they matter, especially if you’re seeking specialized trauma therapy, and how our collaboration with Mentaya makes the process easier.
What Are Out-of-Network Benefits?
Out-of-network benefits are part of many insurance plans that reimburse you for seeing providers who aren’t in your insurance company’s contracted network. Instead of being restricted to a narrow directory, OON benefits give you freedom to choose a therapist who best fits your needs—whether that’s advanced trauma training, cultural attunement, or flexible scheduling.
Here’s how it usually works:
- You pay your therapist directly for sessions.
- You (or a platform like Mentaya) submit a claim to your insurance company.
- Your insurance reimburses you a portion of the cost, depending on your plan.
Why Out-of-Network Benefits Matter
Therapy is not one-size-fits-all. Finding the right therapist, someone who understands your experiences and specializes in your needs, makes all the difference. Sometimes, the right fit simply isn’t listed in your insurance company’s directory.
At our practice, what sets us apart is our specialized trauma therapy. While many directories list providers broadly under “therapy” or “counseling,” they don’t always show who has advanced training in trauma-focused approaches such as:
- EMDR (Eye Movement Desensitization and Reprocessing)
- Internal Family Systems (IFS)
- Polyvagal-informed therapy
- Integrative trauma-focused approaches
These methods require years of training and supervision, and they’re not always easy to find in-network. Insurance panels often prioritize filling provider slots quickly over curating specialized expertise. That’s why your out-of-network benefits can be a lifeline: they give you the flexibility to choose a therapist with the expertise you truly need.
Specialized Trauma Therapy: Why It’s Worth the Investment
Healing from trauma is not about quick fixes. It’s about safe, tailored, and evidence-based care. At our practice, we specialize in helping clients move beyond survival mode into healing and growth through trauma-informed approaches.
Unfortunately, in-network directories don’t always guarantee this level of care. That’s why investing in specialized trauma therapy, even if it means using your OON benefits, is so valuable. Your healing deserves more than “what’s available.” With out-of-network coverage, you can access care that is transformational rather than transactional.
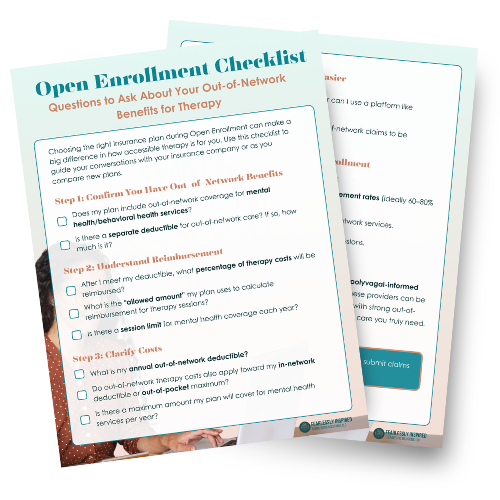
Open Enrollment: Why This Timing Matters
We’re approaching Open Enrollment season—the window when you can review, renew, or switch your health insurance plan. This is the perfect time to make sure your plan supports your mental health goals.
When reviewing your options, pay close attention to mental health coverage, especially for out-of-network care:
- Look for plans with strong out-of-network mental health benefits.
- Ask about deductibles and how much you must pay before reimbursement begins.
- Review what percentage of therapy costs are reimbursed after the deductible.
- Compare the allowed amounts (the maximum your insurance will reimburse per session).
If your mental health is a priority, choosing a plan with robust OON benefits ensures you’re not locked out of the care you need—especially when seeking specialized therapy.
Making It Easier with Mentaya
We know that navigating insurance claims can feel overwhelming. That’s why we’ve partnered with Mentaya, a platform designed to take the stress out of using your out-of-network benefits.
With Mentaya:
- Claims are submitted directly to your insurance company on your behalf.
- Reimbursement is tracked, with follow-ups handled as needed.
- You save time, avoid confusing paperwork, and focus on your healing.
By working with Mentaya, we ensure you don’t leave money on the table when it comes to your mental health care.
How to Start: Checking Your Benefits
Many people don’t realize they already have OON benefits. The first step is understanding what your plan covers. When checking your plan:
- Look for sections labeled “Behavioral Health” or “Outpatient Mental Health Services.”
- Confirm if you have an out-of-network deductible (and how much it is).
- Find out what percentage of therapy costs are reimbursed after your deductible.
- Ask about the allowed amount your insurance company uses for reimbursement.
If you’re choosing a new plan during Open Enrollment, prioritize options that provide strong out-of-network coverage. This ensures flexibility and peace of mind when it comes to accessing specialized care.
The Bottom Line
Out-of-network benefits open the door to therapy that might otherwise feel out of reach. If you’ve been putting off therapy because you assumed insurance wouldn’t cover it, now is the time to look again.
- Review your plan for out-of-network mental health coverage.
- Take advantage of Open Enrollment to choose a plan that supports your goals.
- Let Mentaya handle the reimbursement process so you can focus on healing.
Your mental health is too important to settle for generic care. With out-of-network benefits, you don’t have to. You can access specialized trauma therapy—safe, effective, and deeply healing.
Ready to begin or have questions about using your benefits with us? Reach out today. We’ll walk you through the process so you can focus on what matters most: your healing and growth.